Ocular hypertension and glaucoma
Not all the people who have ocular hypertension will develop glaucoma, not all people with high blood pressure will develop glaucoma.
Nor is arterial hypertension the same as ocular hypertension and the relationship with glaucoma may or may not be correlative. Identifying this causality is vital to establish a treatment regimen.
Ocular hypertension and glaucoma
Not all the people who have ocular hypertension will develop glaucoma, not all people with high blood pressure will develop glaucoma.
Nor is arterial hypertension the same as ocular hypertension and the relationship with glaucoma may or may not be correlative. Identifying this causality is vital to establish a treatment regimen.
Relationship between glaucoma and ocular hypertension
El Glaucoma is defined as an optic neuropathy progressive multifactorial cause, where one of the most important risk factors is High intraocular pressure.
With this definition we are pointing out that ocular hypertension, depending on their values and duration time, will cause damage to the optic nerve. When this alteration occurs, then we speak of glaucoma.
We know that the ocular hypertension, which has nothing to do with arterial systemic hypertension, the higher and longer it acts, with higher probability of that ends up generating a glaucoma.
However, not all glaucomas are caused by ocular hypertension, although it is no less true that the majority of glaucomas appear in eyes affected by ocular hypertension.
Is ocular hypertension the same as glaucoma?
Not all ocular hypertensives develop glaucoma (involvement of the optic nerve), not all ocular normotensive is exempt from the risk of suffering from glaucoma.
Intraocular pressure and glaucoma
El glaucoma is one of the leading causes of blindness in the world, which defines it as A serious illness. One of the biggest problems we have with glaucoma is that does not usually cause discomfort until stages of the disease in which a partial loss of vision, with irreversible character, so its early diagnosis is difficult to perform.
Until recently diagnosed with glaucoma a patient on a routine examination taking intraocular pressure. If the pressure was high, more tests were done and a diagnosis was made. However, we have seen that, although the taking intraocular pressure is a first step, does not help us much, since there are glaucomas that course with normal pressure, Normotensional glaucomas, and patients who due to other factors such as corneal thickness, the values of the intraocular pressure, they are not real, are falsified and may be elevated or decreased, a more serious situation because if more tests are not done, this possible glaucoma will go unnoticed.
Today it is still difficult for us to accurately predict the value of Intraocular Pressure (IOP) that causes damage to the optic nerve.
Ocular hypertension and glaucoma
How can we know if a patient with ocular hypertension has high risk of developing glaucoma?
- On the one hand we must rely on a complete eye examination, with special emphasis on the aspect of the optic nerve.
- On the other hand we must value the family and personal history.
- Support us in new technologies and diagnostic machinery that increasingly try to bring us closer to early diagnosis or risk of suffering from glaucoma.
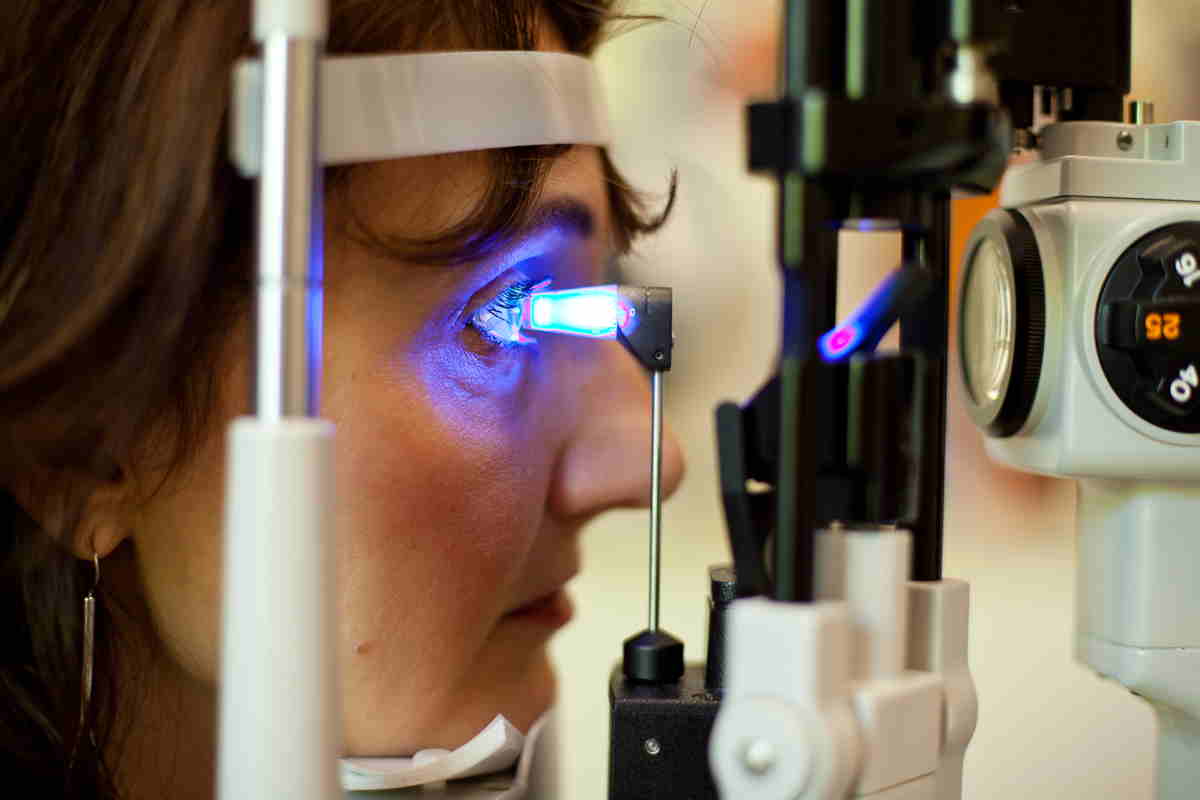
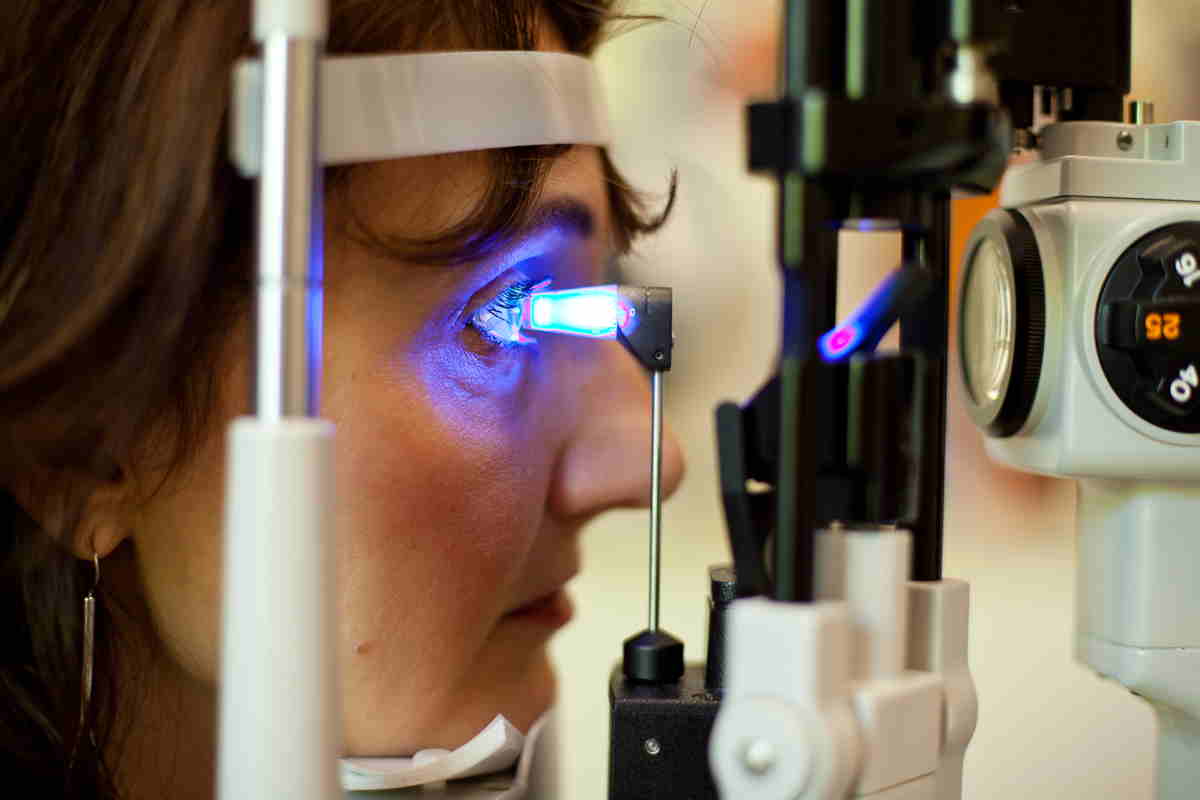
Complete ophthalmologic examination
In a eye examination we must measure:
- measurement of the Intraocular pressure: Considered interval of normal values Between 18-21mm HG.
- Corneal thickness (Pachymetry): Pachymetries with low values can give values of lower than real intraocular pressure and a high value of corneal thicknesscan give high IOP values that induce think it's about of a glaucomatous hypertension.
- Appearance of the papilla: Generally, when we detect morphological changes at the papilla level, glaucoma is already established.
family and personal history
The family history of glaucoma, and la myopia, diabetes, afro-american race, etc., are factors to take into account in order to assess the risk of glaucoma.
Diagnostic machinery
Currently requires a series of instruments to highlight possible eye injuries related to glaucoma.
En Área Oftalmológica Avanzada we have the necessary technological means to be able to assess not only the degree of glaucoma and its progression, but also the risk of suffering glaucoma, using special techniques of early diagnostic.
Diagnosis of glaucoma with ocular hypertension
In this section we highlight the importance of using pruebas diagnostic for power to diagnose precisely those glaucomas in patients with ocular hypertension.
Among them we highlight:
Gonioscopy
It serves to divide glaucomas into the two large groups, namely, closed angle o open angle.
Nowadays we also have the OCT anterior chamber to measure angle and discriminate these two types of glaucoma.

Retinography
Retinography is a photograph taken at the fundus of the eye that lets study carefully the papilla morphology y appreciate small splinter hemorrhages.

ORA
The ORA is responsible for measuring intraocular pressure adjusted by corneal biomechanics.
Allows us assess intraocular pressure based on pachymetry and corneal elasticity.
Computerized perimetry ocampor visual
The complementary ophthalmological examination that studies the alteration of the campor visual.
The campo visual analyzes and quantifies the sensitivity of the retina to different light stimuli that vary in intensity, size and location. Of fundamental importance in the diagnosis and follow-up of patients with glaucoma.
Although it represents a great advance in the diagnosis of glaucoma, only detects alterations from a loss of 40% of retinal ganglion cells, too late to be the only instrument to prevent visual loss.
For this reason, other techniques based on perimetry for the early detection, such as strategies based on shortwave stimuli, blue, on yellow background.
FDT dual frequency analyzer
Based on the selective damage theory and the redundancy theory, the FDT seeks to highlight the specific damage to the nerve fibers of the retina and optic nerve that conduct the motion vision signal.
Various experiences showed that in glaucoma these types of nerve fibers were damaged earlier, so a method was sought that could reveal their alteration.
The Dual Frequency FDT Analyzer allows studying the magnocellular pathway. It is a test that takes less time than a campimetry normal, minor level of patient care y enjoys greater sensitivity y specificity.
Optic nerve injuries are manifested with 20% damage, compared to 40% what was necessary in the campclassical symmetry, which represents a great advance in early diagnosis.
GDX Laser Polarimetry
El GDX study the nerve fiber layer thickness (CFNR), measuring the delay in the beam of a polarized laser, induced by the birefringent microtubules of the axons of the ganglion cells.
Analyzes a strip of the peripapillary RNFL and offers various maps and parameters. Included in the nerve fiber indicator and the relative parameters is the curve that represents the thickness of the nerve fiber layer, TSINT curve.
EL GDX detects lesions from 10% of involvement of the optic nerve.
OCT of papilla and ganglion cells
El OCT for glaucoma with ocular hypertension our lets studyboth quantitatively and qualitatively, the changes that occur in this layer at the level of the peripapillary retina. It also provides morphometric and topographic information on the state of the optic nerve head.
The cape ganglion cells in the macular region indicates significant structural changes for the early diagnosis of glaucoma.
Detection of injuries from 15% of involvement of the optic nerve.
Transmission
Between the glaucoma treatments with ocular hypertension we find the classic ones with instillation of drops to control intraocular pressure, the application of YAG laser or the glaucoma surgery.
The criteria for starting treatment of a patient with galaucoma with ocular hypertension are as follows:
Is considered high risk patient and needs treatment if:
- Presents defects in layer of retinal nerve fibers.
- Parapapillary changes.
- Intraocular pressure greater than 30 mm Hg.
Factors of moderate risk:
- Intraocular pressure 24-29 mm Hg flawless in layers of nerve fibers.
- Family history de Glaucoma primary of open angle (POAG).
- High myopia.
- Excavation ratio –Vertical disk greater than 0.7
Factors of Low risk:
- Intraocular pressure 22-24 mm Hg.
Follow-up of glaucoma in a person with ocular hypertension
In a patient with ocular hypertension at risk of glaucoma, first visit it is advisable to perform the following diagnostic tests:
- Pachymetry
- ORA
- FDT
- OCT ganglion cells and papilla
- GDX
Depending on the results we obtain from the diagnostic tests, we will follow the following guidelines:
In patients of high risk or moderate risk it's recommended review every 6 months.
patients of low risk requires a semi-annual or annual review, according to the medical history.
The timing of the controls is always related to the evolution of the disease associated with each case.